Preparing For MIPS 2024
Get ready for MIPS 2024 with these essential tips and strategies to maximize your performance and succeed in the program.

On November 2, 2023, the Centers for Medicare and Medicaid Services (CMS) released the 2024 Medicare Physician Fee Schedule (PFS) Final Rule, which includes updates to the Quality Payment Program (QPP) and explains the CMS Payment and Policy Changes. This blog summarizes the key policy changes affecting the traditional Merit-based Incentive Payment System (MIPS) program. While wrapping up your 2023 MIPS reporting should be a priority, it’s also important to stay informed of the upcoming changes that will impact your reporting during the 2024 performance year.
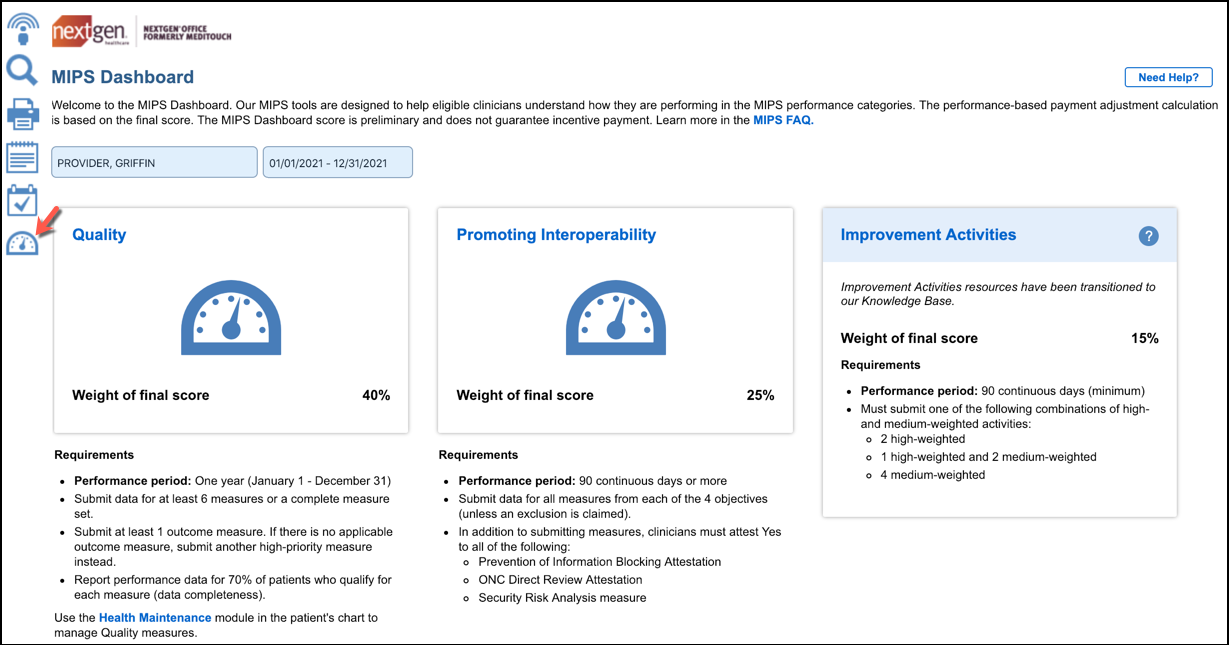
As a refresher, traditional MIPS comprises four performance categories: Quality, Cost, Promoting Interoperability (PI), and Improvement Activities (IA). A provider’s score for each of these categories determines one’s total MIPS score and corresponding payment adjustment.
Performance Category Weights
For the 2024 performance year, the Quality, Cost, IA, and PI performance category weights will remain the same as in 2023:

CMS did not finalize the proposal to increase the performance threshold so it will remain at 75 points for the 2024 performance period (the same as the 2023 performance year). Final MIPS scores are compared to the performance threshold to calculate the MIPS payment adjustment.
The table below breaks down final MIPS scores and their associated payment adjustments based on the performance threshold.
| 2024 Performance Period | |
|---|---|
|
2024 Final MIPS Score |
2026 MIPS Adjustment |
| 0.0-18.75 | Negative 9% |
| 18.76-74.99 | Negative MIPS payment adjustment greater than negative 9% and less than 0% on a linear sliding scale |
| 75.0 | 0% adjustment |
| 75.01-100 | Positive MIPS payment adjustment greater than 0% on a linear sliding scale. The linear sliding scale ranges from 0 to 9% for scores from 75.00 to 100.00 This sliding scale is multiplied by a scaling factor greater than zero but not exceeding 3.0 to preserve budget neutrality. |
Clinicians must meet “data completeness” when reporting Quality measures to ensure that the data submitted is sufficient to assess quality performance. CMS previously finalized a 75% data completeness threshold for the MIPS 2024 and 2025 performance periods (up from 70% in 2023) for electronic Clinical Quality Measures (eCQMs), MIPS CQMs, Medicare Part B claims measures, and QCDR measures. This means that Quality measures must be reported on a minimum of 75% of eligible instances for the entire year.
CMS did not finalize the proposal to increase the data completeness threshold for reporting quality measures in the 2027 performance period. The data completeness threshold will remain at 75% through the 2026 performance period.
There are a total of 198 quality measures for the 2024 performance period which reflect:
CMS also finalized the addition/removal of 2 radiology measures with a one-year delay:
A list of new measures, along with their collection types, are outlined in the table below.
| New Quality Measures | Collection Type |
|---|---|
| #495 Ambulatory Palliative Care Patients’ Experience of Feeling Heard and Understood | MIPS CQM |
| #496 Cardiovascular Disease (CVD) Risk Assessment Measure - Proportion of Pregnant/Postpartum Patients that Receive CVD Risk Assessment with a Standardized Instrument | MIPS CQM |
| #497 Preventive Care and Wellness (composite) | MIPS CQM |
| #500 Connection to Community Service Provider | MIPS CQM |
| #501 Appropriate Screening and Plan of Care for Elevated Intraocular Pressure Following Intravitreal or Periocular Steroid Therapy | MIPS CQM |
| #502 Acute Posterior Vitreous Detachment Appropriate Examination and Follow-up | MIPS CQM |
| #503 Acute Posterior Vitreous Detachment and Acute Vitreous Hemorrhage Appropriate Examination and Follow-up | MIPS CQM |
| #504 Improvement or Maintenance of Functioning for Individuals with a Mental and/or Substance Use Disorder | MIPS CQM |
| #505 Gains in Patient Activation Measure (PAM®) Scores at 12 Months | MIPS CQM |
| #506 Initiation, Review, And/Or Update To Suicide Safety Plan For Individuals With Suicidal Thoughts, Behavior, Or Suicide Risk | MIPS CQM |
| #507 Reduction in Suicidal Ideation or Behavior Symptoms | MIPS CQM |
A list of measures that have been removed or partially removed is outlined in the table below.
| Retired Quality Measures | Collection Type |
|---|---|
| #14 Age-Related Macular Degeneration (AMD): Dilated Macular Examination | MIPS CQM |
| #93 Acute Otitis Externa (AOE): Systemic Antimicrobial Therapy – Avoidance of Inappropriate Use | MIPS CQM |
| #107 Adult Major Depressive Disorder (MDD): Suicide Risk Assessment | eCQM |
| #110 Preventive Care and Screening: Influenza Immunization | Medicare Part B Claims, eCQM, MIPS CQM |
| #111 Pneumococcal Vaccination Status for Older Adults | Medicare Part B Claims, eCQM, MIPS CQM |
| #138 Melanoma: Coordination of Care | MIPS CQM |
| #147 Nuclear Medicine: Correlation with Existing Imaging Studies for All Patients Undergoing Bone Scintigraphy | Medicare Part B Claims, MIPS CQM |
| #283 Dementia Associated Behavioral and Psychiatric Symptoms Screening and Management | MIPS CQM |
| #324 Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Testing in Asymptomatic, Low-Risk Patients | MIPS CQM |
| #391 Follow-Up After Hospitalization for Mental Illness (FUH) | MIPS CQM |
| #402 Tobacco Use and Help with Quitting Among Adolescents | MIPS CQM |
| Quality Measures Removed from Traditional MIPS* | Collection Type |
| #112: Breast Cancer Screening | Medicare Part B Claims, eCQM, MIPS CQM |
| #113: Colorectal Cancer Screening | Medicare Part B Claims, eCQM, MIPS CQM |
| #128: Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-up Plan | Medicare Part B Claims, eCQM, MIPS CQM |
*These measures would still be available for MVP reporting. Quality measures 112 and 113 would also be maintained for the CMS Web Interface collection type available to Shared Savings Program ACOs reporting through the APP.
Check Out the NextGen Office MIPS Dashboard
There are 106 Improvement Activities in the MIPS inventory for 2024, including five new activities and the removal of three existing improvement activities as outlined in the table below:
| New Improvement Activities | Retired Improvement Activities |
|---|---|
| IA_PM_22 Improving Practice Capacity for Human Immunodeficiency Virus (HIV) Prevention Services Guidelines (submitted by CDC) | IA_BMH_6 Implementation of co-location PCP and MH services |
| IA_MVP Practice-Wide Quality Improvement in MIPS Value Pathways | IA_BMH_13 Obtain or Renew an Approved Waiver for Provision of Buprenorphine as Medication-Assisted Treatment [MAT] for Opioid Use Disorder |
| IA_PM_23 Use of Decision Support to Improve Adherence to Cervical Cancer Screening and Management | IA_ PSPA_29 Consulting Appropriate Use Criteria (AUC) Using Clinical Decision Support when Ordering Advanced Diagnostic Imaging |
| IA_BMH_14 Behavioral/Mental Health and Substance Use Screening & Referral for Pregnant and Postpartum Women | |
| IA_BMH_15 Behavioral/Mental Health and Substance Use Screening & Referral for Older Adults |
Beginning in 2024, the performance period for the PI Category will increase from a minimum of 90 continuous days to a minimum of 180 continuous days within the calendar year.
The definition of Certified Electronic Health Record Technology (CEHRT) is updated to
align with the Office of the National Coordinator for Health IT (ONC) regulations which move away from the “edition” construct for certification criteria. References to the “2015 Edition health IT certification criteria” will be replaced with “ONC health IT certification criteria”.
CMS is discontinuing automatic reweighting for the following clinician types beginning in 2024:
The agency plans to continue automatic reweighting for the following clinician types in the 2024 performance period:
Query of Prescription Drug Monitoring Program (PDMP) Measure Exclusion - CMS has modified the current exclusion for the Query of Prescription Drug Monitoring Program (PDMP) Measure to accommodate clinicians who don’t electronically prescribe any Schedule II opioids and Schedule III and IV drugs during the performance period.
Safety Assurance Factors for EHR Resilience (SAFER) Guides Measure - A “yes” response is required to fulfill the SAFER Guide measure beginning with the MIPS 2024 performance period.
The calculation for the Cost improvement score is updated to ensure that improvement in the Cost category is more accurately scored and aligns with the Quality category scoring improvement methodology. Beginning with the 2023 performance period, the improvement scoring for the Cost category will be calculated at the category level without using statistical significance.
A maximum Cost improvement score of one percentage point out of 100 percentage points is established beginning with the 2023 performance period and a maximum Cost improvement of zero percentage points for the 2022 performance period.
In 2024 there will be a total of 29 Cost measures available for CMS to calculate a Cost score. Five new episode-based cost measures are added for the 2024 performance period:
The acute inpatient medical condition measure Simple Pneumonia with Hospitalization has been removed for 2024 due to coding changes.
CMS is delaying the removal of the CEHRT threshold requirements for Shared Savings Program ACOs by one year. Beginning with the 2025 performance year, CMS will require that all MIPS eligible clinicians, Qualifying APM Participants (QPs), and Partial QPs participating in an ACO, regardless of track, must be on CEHRT. ACOs will have to satisfy all of the following requirements unless otherwise excluded:
How Can We Help?
AVS Medical offers MIPS Consulting Services to our NextGen Office Users. Find out more about our consulting service and let us assist and educate you in meeting all of the necessary requirements for MIPS 2024
Get ready for MIPS 2024 with these essential tips and strategies to maximize your performance and succeed in the program.
NextGen Office EHR/PM is now interfaced directly to CMS’s QPP site. Our latest release features an interface to the CMS Quality Payment Program or...

Healthcare delivery is changing, and the technology that has enabled providers to offer a virtual, contactless experience is here to stay. An...