An Electronic Prior Authorization (EPA) is an electronic version of the paperwork sent in a secure format to PBMs and pharmacies. CoverMyMeds offers electronic connections and workflows to submit Prior authorizations to insurance companies and pharmacies without having to use paper. Their service covers payers with available electronic connections and also offers the ability to digitally fax PBMs that are still using paper to process prior authorizations.

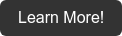
The NextGen Office partnership with CoverMyMeds allows providers to send prospective ePAs to pharmacies and insurance companies from within the NextGen Office Application. The prospective workflow is the act of a provider and their staff initiating an ePA before sending the medication to the pharmacy. This avoids providers having to send ePAs after the medication has reached the pharmacy and decreases the amount of time a patient has to wait for a medication requiring prior authorization. The integration with CoverMyMeds will save the providers and their staff time while also providing a better patient experience.
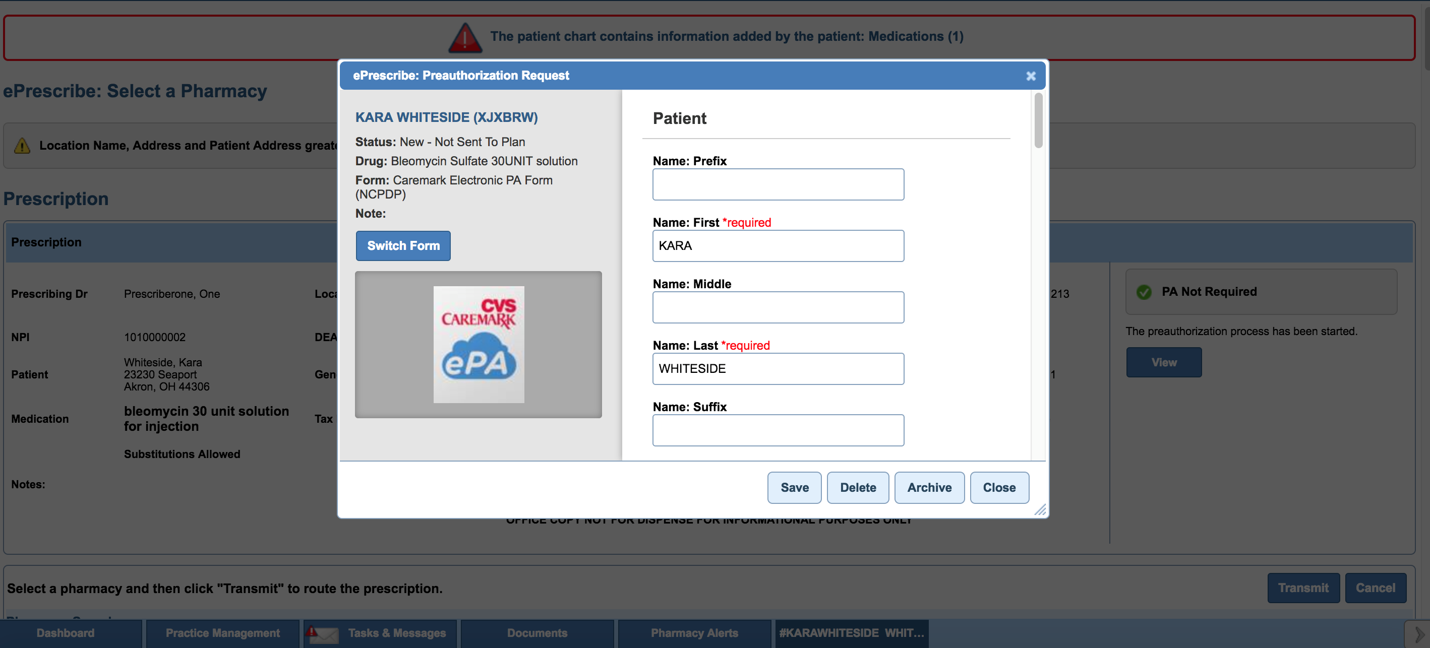
A typical Prior Authorization takes about 20 minutes and 3-5 business days through a manual process. Utilizing an ePA can reduce this to a 5 minute process and 1-2 business days and will help reduce time to therapy for the patient. This will also increase the likelihood that the patient will pick up the medication(s) they need to live a healthier life.
- 1 in 20 Electronic Medications require a pre-authorization
- Common workflow in many offices
- Helps with Patient Satisfaction, Physician Burnout, and Staff Satisfaction
The CoverMyMeds Integration is also free of charge. It will be released and available to all NextGen Office clients who choose to use the workflow.
For more information on How CoverMyMeds Integration works, take a look at our brief Presentation HERE!
Interested in NextGen Office?